Understanding Anticholinergics
In today’s video, I break down the one category of medications -- Anticholinergics -- that research consistently links to cognitive decline especially in adults over 50.
HeartFood.Blog
12/20/20259 min read
316,174 views Nov 26, 2025
🧠 Get The Dangerous Dementia Drugs Guide for FREE here: https://subscribepage.io/dangerous-de...
Get The Best & Most Affordable Magnesium Glycinate On Amazon: https://lvnta.com/lv_NPFSO28kPs4efLmmdn
📊 Get The Smart Symptom Spreadsheet for FREE here: https://subscribepage.io/smart-sympto...
Are some of the most common medications actually increasing your risk for memory loss and dementia?
In today’s video, I break down the one category of medications -- Anticholinergics -- that research consistently links to cognitive decline especially in adults over 50.
This is not about fear — it’s about empowerment.
Most people have no idea this link exists, and it’s one of the biggest hidden issues I see in my clinic.
If you’re on these medications, watch this before your next refill!
Video Time Stamps:
0:00 Intro
1:01 What Is This Class of Medications?
2:06 Specific Medication Examples
2:55 What The Research Shows
3:41 Who's Most At Risk?
5:28 SAFER Alternatives
7:20 The BEST Thing You Can Do For Your Brain
Vitals & Voices: https://www.skool.com/vitals-voices-2... — my free, private, doctor-led community for people who want deeper answers, smarter conversations, and a space to ask real health questions without judgment
🩺 The Weekly Checkup: dr-mitch-rice.kit.com/theweeklycheckup — my free email newsletter packed with symptom spotlights, lab insights, doctor-approved tools, and real stories from people just like you. All in one clear email, once a week. 🌐 All My Resources + Website: dr-mitch-rice-f4tq6y.mailerpage.io

Anticholinergic Side Effects in the Older Adult Population
Medications with anticholinergic activity have a wide range of physiological effects and are useful in treating a variety of medical conditions that are common in the older adult population.
However, older adults are especially susceptible to the adverse effects of anticholinergic medications which can lead to serious physical and mental impairment.
What Does Anticholinergic Mean?
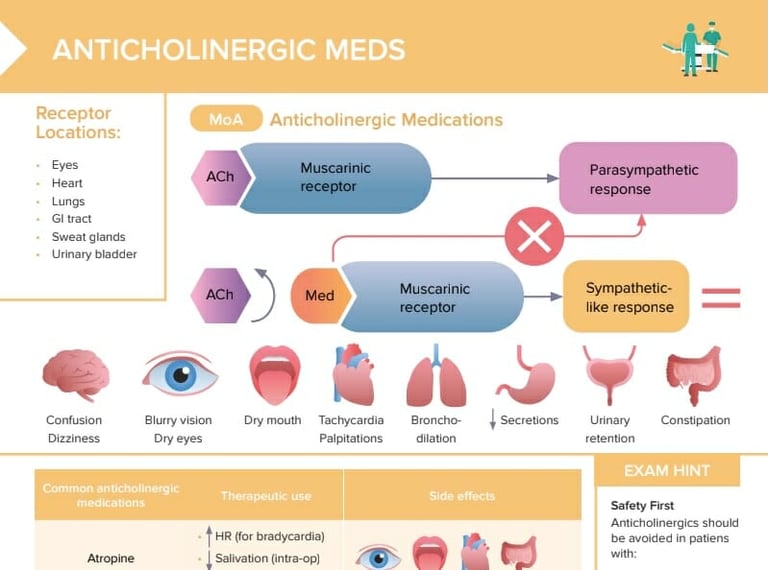
Anticholinergic is defined as opposing or blocking the physiologic actions of acetylcholine.
Acetylcholine is a neurotransmitter utilized by both the central and peripheral nervous systems.
Anticholinergic medications act as antagonists to reduce or prevent the effects of acetylcholine at nicotinic and/or muscarinic receptor sites.
What are Anticholinergic Drugs Used to Treat?
Anticholinergic drugs have effects on respiration, circulation, vision, alertness, and more.
Drugs with anticholinergic activity are useful for treating several conditions including:
Allergies
Asthma
Cardiovascular disease
Chronic obstructive pulmonary disease (COPD)
Mydriasis
Parkinson’s disease
Urge incontinence
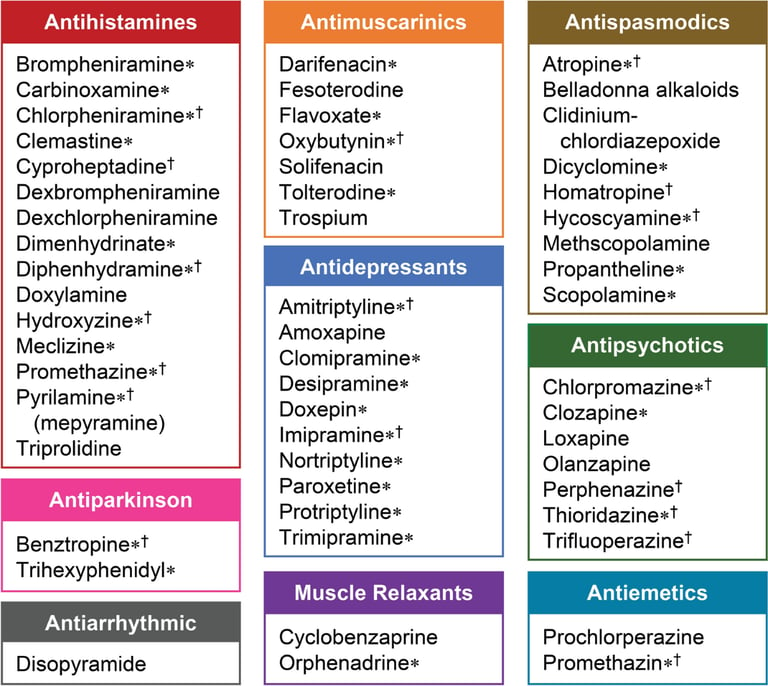
While anticholinergic medications are therapeutic for many conditions, countless medications possess anticholinergic properties that are not responsible for their therapeutic effects and increase the risk of adverse events.
This includes the antipsychotics, tricyclic antidepressants, diphenhydramine, and more.
What are the Adverse Effects of Anticholinergic Drugs?
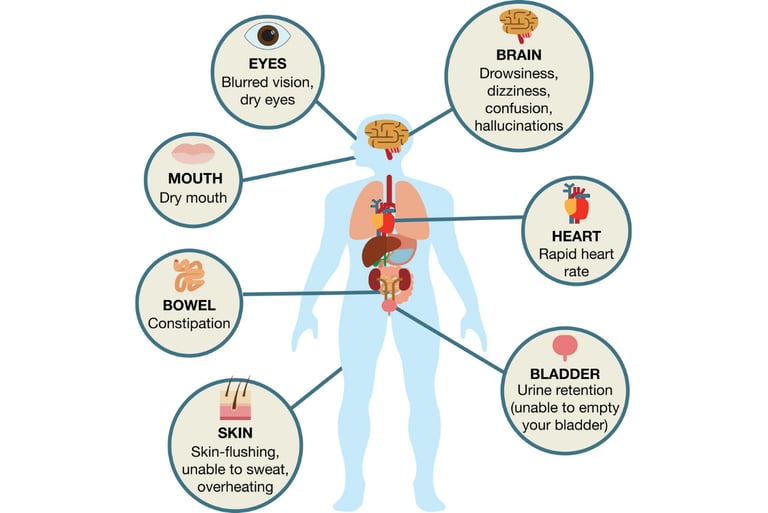
The adverse effects of anticholinergic drugs are divided into central and peripheral effects.
Medications that are able to more readily cross the blood-brain barrier have an increased likelihood of causing central adverse effects.
Central anticholinergic adverse effects may include:
Attention deficit
Confusion
Impaired concentration
Memory impairment
Common peripheral anticholinergic adverse effects may include:
Blurred vision
Constipation
Decreased sweating
Dilated pupils
Dry mouth
Tachycardia
Urinary retention
Additionally, many conditions that are common in the older adult population are negatively impacted by anticholinergic medications.
This includes dementia, hyperthyroidism, glaucoma, prostate hypertrophy, tachyarrhythmia, and more.
According to the AGS Beers Criteria, the main risk rationale for avoiding or minimizing anticholinergic drugs in older adults is due to the increased risk of cognitive decline.
But how exactly do we know the likelihood of individual drugs and drug combinations for causing these adverse effects and risks?
What is the Anticholinergic Burden?
The anticholinergic burden is the cumulative effect of using multiple drugs with anticholinergic activity together.
Dr. Malaz Boustani, a researcher at the Indiana University Center for Aging Research, and her colleagues developed a scale called Anticholinergic Cognitive Burdern (ACB) Scale to provide clinicians with practical guidance for using anticholinergic medications in older adults.
Studies that utilized the ACB scale have demonstrated that higher anticholinergic burden predicts cognitive impairment in older adults.
According to a recent systematic review that identified 19 anticholinergic burden scales and 104 validation studies, the ACB scale achieved the highest percentage in quality.
The ACB scale categorizes anticholinergic medications on a scale of 0 to 3:
ACB score 0 means no anticholinergic effect
ACB score 1 represents possible anticholinergic effect but no clinically relevant negative cognitive effects
ACB scores 2 and 3 mean definite anticholinergic effect, with a score of 3 being based on blood-brain barrier permeability and association with the development of delirium
The total added score of different drugs determines the accumulative ACB.
Anticholinergic burden should also take into account dosing and potency of medications.
If anticholinergic drugs need to be used in older adults, they should be used at the lowest doses for the shortest time possible.
An Opportunity for Personalized Medicine
Prescription and nonprescription medications need to be used with special caution in the older adult population because of the anticholinergic burden, age-related changes in pharmacokinetics, comorbid conditions, drug interactions, and more.
Pharmacogenetic (PGx) testing provides additional insight into a patient’s individual drug metabolism profile.
This insight can help healthcare providers develop a more patient-specific treatment plan.
For example, consider amitriptyline which has an ACB score of 3.
Amitriptyline has specific dosage adjustments for CYP450 poor metabolizers.
The FDA Table of Pharmacogenomic Biomarkers in Drug Labeling specifically cites “…poor metabolizers have higher than expected plasma concentrations of tricyclic antidepressants (TCAs) when given usual doses.
Depending on the fraction of drug metabolized by CYP2D6, the increase in plasma concentration may be small, or quite large (8 fold increase in plasma AUC of the TCA)”.9
In addition, the Clinical Pharmacogenetics Implementation Consortium (CPIC) provides further dosing recommendations for TCAs based on CYP2D6 and CYP2C19 phenotype.
According to the CPIC Guideline, amitriptyline use should be avoided in a 2D6 poor metabolizer but if use is warranted, consider a 50% reduction of the recommended starting dose.10
In order to help clinicians navigate the available pharmacogenetic guidelines, Genomind provides clinicians with access to GenMedPro, an outstanding tool to help evaluate both gene-drug and drug-drug interactions, pharmacogenetic guideline recommendations, and alternative medication options, as appropriate.
GenMedPro™ can help providers be more informed before prescribing these drugs in older adults if there is additional risk (i.e. increased drug exposure).
To learn more about GenMedPro™ or to request a demonstration from our PhD and PharmD experts, please utilize Genomind’s Clinician Portal.
Are You Ready to Upgrade Your Practice with Genomind?
Genomind's pharmacogenetic testing is the most advanced and comprehensive mental health pharmacogenetic test available.
Get access to 26 genes related to mental health, 130+ medications, 10+ conditions, state-of-the-art tools, and 360 degrees of support. Register today.
Transcript
Every day, millions of people take medications for anxiety, allergies, sleep, or
bladder problems, thinking they're harmless.
But what most people don't realize is that many of these medications are quietly
increasing their risk of dementia.
And they're even changing how the brain itself functions.
In fact, taking just one of these medications daily for a year can increase the risk of
getting dementia by 50%.
And research shows they can cause brain shrinkage and memory loss over time.
And the craziest part is that these aren't rare or experimental drugs.
They're sitting in medicine cabinets everywhere and they might just be in yours.
By the way, I'm Dr. Mitch Rice, a practicing boardcertified family medicine
physician with a focus on integrative care.
And today I'm going to break down the specific medications that are damaging
your brain long term, the science behind how they work, and the safer
alternatives you can start using today instead.
So, let's start with the basics.
The class of medications that we're talking about today is called antiolinerics.
And that word just means they block a certain chemical in your brain known as
acetylcholine.
Imagine your brain as a city filled with communication wires.
Acetylcholine is like the electrical current that powers those wires and allows the
neurons to talk with one another.
Antiolineric medications block that current and weaken connections between
memory centers in the brain like the hippocampus and the cerebral cortex.
Over time, those connections fade, leading to brain shrinkage and slower
processing speeds.
Antiolineric effects show up in tons of medications, both prescription and
non-prescription. A few of the most common examples are allergy medications
like dyenhydramine also known as benadryil and other older antihistamine
medications.
Sleep aids such as Tylenol PM or Zquil.
Anxiety medications like hydroxazine also known as Viststeril or Addterax.
Bladder control medications like Ditropan and Vesicare.
Irritable bowel syndrome or IBS medications like Bentil.
Motion sickness medications like Dramamine and Scopalamine.
Each one of these medications alone blocks acetylcholine and the more you take,
the bigger the impact.
And this isn't just theory. It's literally been studied over and over again.
A metaanalysis of 1.5 million people found that long-term antiolineric use was an
independent risk factor for both Alzheimer's disease and all cause dementia.
Another study of 21 separate trials showed that taking these meds for just 3
months increased dementia risk by 46% on average.
And brain imaging studies from Jamon Neurology revealed that people using
antiolinerics had increased brain atrophy, literally brain shrinkage and reduced
brain metabolism in the memory centers like the hippocampus.
This means your memory starts to fade and your brain becomes less active on
these medications.
So, this isn't just about feeling groggy or foggy.
These medications literally change your brain.
And that change can worsen, especially if you're over the age of 60.
As we mature in life, our natural levels of acetylcholine begin to decline.
So, when you add medications that block it, you're essentially speeding up the
aging process of your brain.
That's why people over the age of 60, especially those who are on multiple
medications, are at highest risk.
I see this all the time in my own practice.
Someone may be taking hydroxazine for some anxiety.
They may be taking some ZQL to help them sleep at night and maybe even some
detactive bladder issues. and they take all of these at once.
Individually, they block a little bit of acetylcholine, but altogether, all of the wires
in the brain don't fire as they're supposed to, and this leads to a decrease in overall
communication. The decrease in communication leads to parts of the brain
shutting down. The higher the antiolineric burden, the higher the dementia risk.
That means if you're on two or more of these medications at the same time, the
risk doesn't just add up, it actually multiplies.
Now, I'm not saying that these medications should never be used.
There's certainly a good time and place to use them, especially in the short term.
If you take benadryil every once in a while for an allergic reaction, or you take a
Zquil to help you get a good night's rest, you'll totally be fine and you're not going
to increase your risk of dementia.
It's when you take these medications day in and day out over a period of months to
years. We really want to try to avoid that from happening. And here's what you
can do instead broken down into two steps. Step one is to go through your
medicine cabinet looking at all of the prescription and the non-prescription
medications. Search online or ask your doctor or even your pharmacist which of
these medications have antiolinergic properties. Step two is don't stop
anything abruptly, especially prescription meds. Talk to your doctor
first about safer alternatives or look up the information yourself online.
Here are a few examples of some safer alternatives that I recommend.
For sleep, try magnesium glycinate, not magnesium oxide or magnesium citrate, as
those cheaper versions of magnesium don't cross into the nervous system as
easily and are more likely to give you an upset stomach.
Magnesium glycinate is a safer option for increasing the quality of your sleep,
much more so than zquil or Tylenol PM.
If you want the best and most affordable version of magnesium glycinate on
Amazon and the one I personally recommend to my patients, I'll put a link in the
description below. For allergy or allergy related issues, use second generation
antihistamines like Claritin, Zerek, and Algra.
These are much less likely to affect your brain long term.
For optimal control of allergies, try switching between these second generation
antihistamines every 3 months.
So if you take Claritin, do that for 3 months, then switch to Zerek for three months,
then Alger for three months, then back to Claritin for three months, etc.
For seasonal allergies, try using nasal sprays like nasal saline or Flonese.
For bladder control, ask about merbbetric, which is a non-antiolineric
option. And for irritable bowel syndrome or IBS, you can try some natural options
like peppermint oil or following a low FODMAP diet.
And most importantly, support your brain with the basics.
Proper sleep, exercise, nutrition, and managing blood pressure, and blood sugar
control will all help prevent brain aging.
Honestly, the number one best thing that you can do in order to prevent dementia
in general is to exercise, as the data shows it to be the most potent anti-brain
aging drug on the market today.
If you've been on these medications for a long period of time, there's no need to
panic, but it is time to act.
The goal of this video is not to scare you, but to empower you.
Because the truth is, many of these brain changes are preventable once you know
what to look for. You deserve to stay sharp, independent, and confident into
your later years, not slowed down by side effects hiding in plain sight.
Dr. Mitch Rice
Healthy Living
© 2026. HeartFood.Blog - All rights reserved.


